The Equity Gap in Pediatric Healthcare
Last week, the LA Times highlighted the ways distance learning exacerbates educational equity issues and shortchanges those from low-income families.
It's clear we must do better.
But this divide doesn’t just impact education. I believe the challenges stemming from poor computers, and broken cell phone connections, pose a threat in a realm that’s gone largely unmentioned: Pediatric Healthcare.
Consider the following:
There are 74mm children in the US, which includes 45mm in low-income families covered by Medicaid or the Children's Health Insurance Program (CHIP). This means that children under the age of 18 make up over roughly 50% of all Medicaid recipients nationwide.
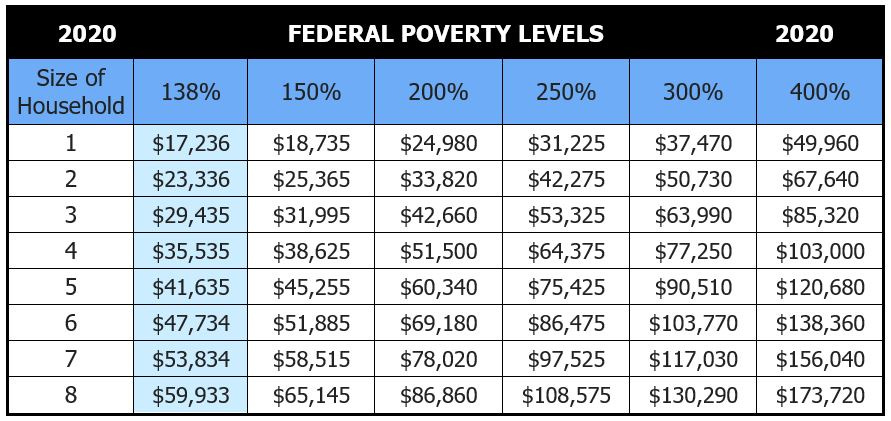
Now picture a family of four, one that needs to make ~$35K a year or less to qualify for Medicaid (138% of the federal poverty level). Families struggling to maintain their income at these levels often can’t find the time during the workday to take their kids in to see a pediatrician or pay for supplementary on-call services. And they most often don't have insurance that extends effective telemedicine solutions to their kids. So, they wait until a time of concern, and resort to taking them to their local 24-hour ER or urgent care facility.
Studies show that Medicaid patients are over 50% more likely than people with commercial health insurance to use the ER as their primary place for care. Yet, one of the biggest drivers of avoidable pediatric Medicaid costs is over-utilization of the ER for non-emergency situations.
For years we've known that having the ER as a pediatric care provider for low-income families is not cost-effective. But what alternatives do they have?
There have been several attempts to fix the ER problem over the years. I wont go into all of them, but telemedicine done right (i.e. purpose built, with features designed for this cohort) has clear potential if aligned with outcomes.
Unfortunately, today, the pediatric needs of the Medicaid population have been largely left behind. Access to technology is just one of the hurdles this group faces. Historically, telemedicine products have been offered through employers as a benefit for employees. This poses a problem for families on Medicaid for two obvious reasons:
First, it’s traditionally been higher-end plans that properly cover and communicate telemedicine benefits, though that's changing. And second, both the product and software workflows are designed for doctors to talk to adults!
As you can imagine, the challenge of pediatrics is that the patients are often veryyoung children. It’s much harder for a doctor to get the information they need to diagnose conditions from them than it is for adult patients.
Thus most vendors and plans have not made pediatric telemedicine a priority because they perceive utilization to be low.
But in reality it may have been just the wrong product. Until now?
As an example, consider Blueberry Pediatrics — a pediatric-focused telemedicine offering that gives parents affordable, quality care instantly via text, phone, or video any hour of the day. Blueberry removes all friction to getting care — there are no appointments, no waiting, and no gatekeepers — at just $15/month.

Any form factor, at any hour is deceptively powerful; it threads the needle on broadband issues and computer access concerns that the LA Times cites. And the Company goes one step further by providing an at-home medical testing kit: parents use the kit to collect their child’s vitals (heart rate, oxygen levels, temperature) and perform ear/nose/throat examinations without leaving home. This means Blueberry can handle cases other telemedicine services can’t, like ear infections, RSV, and croup. It is a powerful wedge, and life-stage to build around.
The best products lead with simplicity. Providing care via text creates significant advantages for the consumer experience as well as the business itself. For example, text messaging also enables physicians to be in constant contact with families and manage symptoms as they progress instead of only getting a single 15-minute snapshot in a video session.
From what I've seen, this is a great step in the right direction, but the world desperately needs more folks like Harrison Gordon and the team at Blueberry building intentional solutions for those in need.
I am not an investor in Blueberry, but I am grateful to my old colleague Adi Sivaraman for introducing me to the team and problem they are solving. I've always believed the best hires teach you, and I was fortunate to hire Adi as an associate years ago; to have him push my thinking on all things healthcare years later is unbelievably rewarding.
We owe it to each other to try and leave no one behind. If your mission is to use technology to better care for a massive, undeserved, segment of the population — get in touch.
Venture capital has a clear role to play and I'd love to help.


Marco, when using the subsidy chart image from Nevada Insurance Enrollment (or any image for that matter), you should always give attribution to the source.
If you do not add attribution, this is your notice to remove the image.